As a defense mechanism, denial has its uses. It can provide a layer of protection – a buffer – between oneself, and the thing that is causing stress and fear to escalate. Having a reprieve from dealing with or accepting the reality of a vulnerable situation can give one time to come to grips and be ready to process. But there is a dark side to denial.
When one becomes rooted in the escape, denial becomes a piece of the problem rather than a protective barrier. Staying planted in denial prevents an individual from addressing the distressing situation and seeking the necessary support to overcome it. Feeling ill-equipped to handle sadness and negative emotions easily leads towards addiction as another means of escaping or mitigating the pressures, vulnerabilities, and fears of one’s reality. In fact, depression and addiction often co-occur.
According to reports from the Journal of the American Medical Association, roughly 50% of individuals diagnosed with a severe mental disorder, and 29% of all individuals diagnosed with a mental illness are also affected by a substance use disorder. Put another way, there are an estimated 9 million adults with both mental health and substance use disorders.
What is more disheartening, is that only around 7% of that staggeringly large number are receiving treatment for both conditions according to the Substance Abuse and Mental Health Services Administration (SAMSHA).
The use of substances to cope with depression is an easy thing to fall into, yet it can lead to a disastrous outcome. The combination of substance use and depression increases the risk of self-inflicted death at an exponential rate. One study found that men who struggle with substances are 2.3 times more likely, and women are 6.5 times more likely to die by suicide.
The trifecta of denial, depression, and addiction creates a dangerous cocktail. To break the cycle, all three elements need to be addressed. Facing problems is essential – which cannot be done when locked tight in the grip of denial. The first step is self assessment.
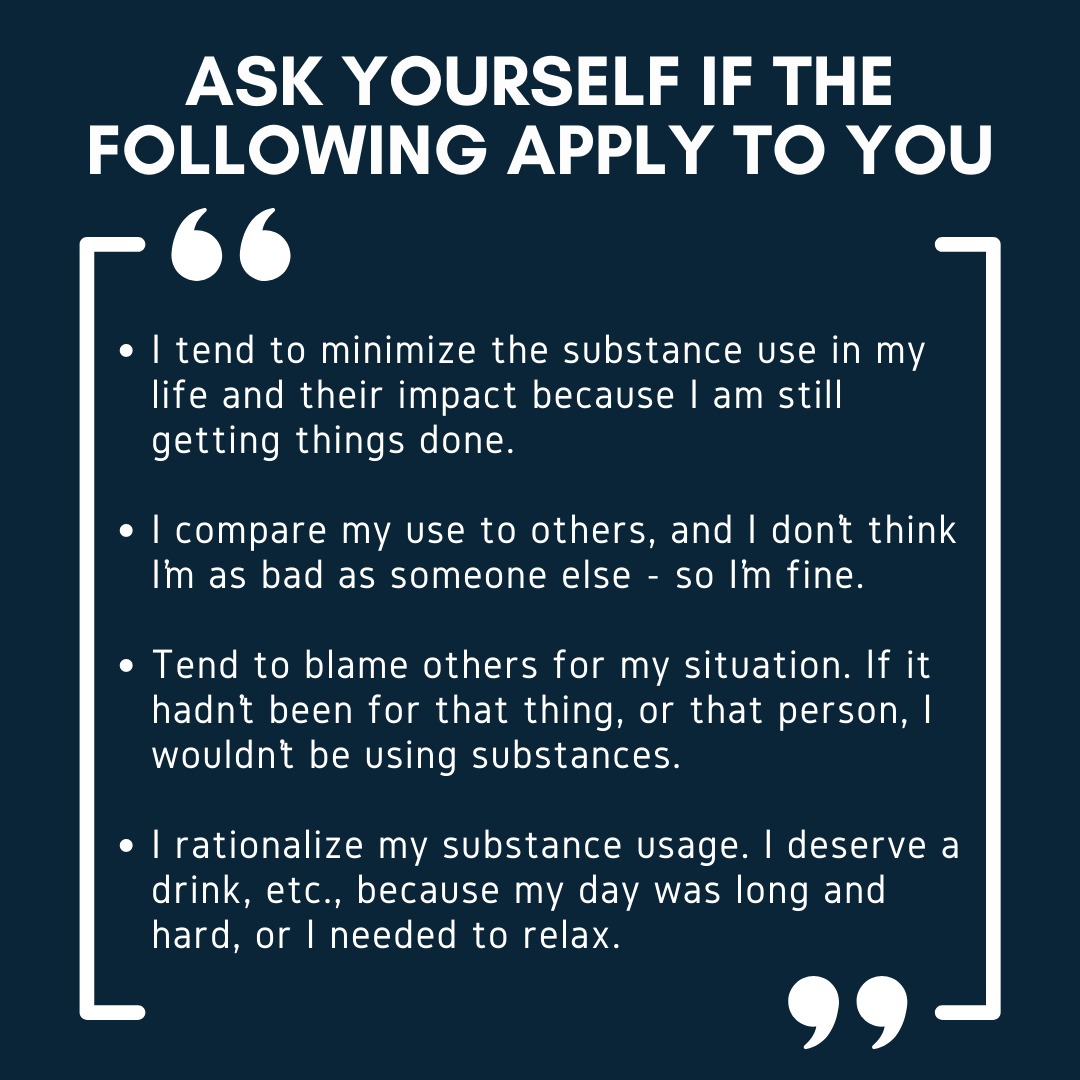
If these statements resonate, denial is in play. When under the heavy weight of depression, this inability to face the reality of a situation will deter further from reaching out for help regardless of its availability. Substance use can also act as a roadblock in the path of mental health treatment, though depression is a key predictive factor of relapse.
Further, ongoing mental health symptoms may become more difficult to manage after addiction due to the neurological changes that occur in the brain after extended substance use.
For more information on the neurological impact of substances, check back for our next blog: Addiction and the Brain
Strategies for overcoming denial
- Examine what you fear.
- Ask yourself what the negative consequences of not taking action might look like.
- Express your fears and emotions.
- Identify irrational beliefs about your situation.
- Journal your experiences.
- Talk to someone you trust.
- Find a support group.
If you are struggling to make progress dealing with a stressful situation on your own, talk to a mental health provider. The struggle is not one that must be faced alone. In fact, we are far more likely to succeed and maintain recovery when supported by a community.
If you think that someone you know is currently in the cycle of denial, depression, and addiction, the best thing you can do is try to be understanding. Support them. Make it clear that you are there for them, care about them, and are concerned while avoiding the use of labels like “alcoholic” and “abuser”. The words we choose to use hold power, and judgement has no place in genuine support.
Supporting sustainable recovery through affordable sober housing solutions is a big part of RCD’s mission. Learn more about RCD’s commitment to community, recovery, and improving outcomes here.
Interested in helping RCD live into their mission? Donate today.